We now live in a world of masks and respirators. It is a world we are not prepared for. The biomedical, sanitary, and technological advances of the last century left us accustomed to breathing freely with little fear of what might be aloft in the air around us.
But because of COVID-19, N95 respirators and cloth masks—their availability and their efficacy—now dominate the news and are at the heart of often vitriolic public debates. Both futuristic and somehow archaic at the same time, millions now depend on their use to prevent infection of a potentially deadly illness.

The respirator and the cloth mask emerged during the nineteenth century and each has been shaped by our shifting understandings of how disease is transmitted within the community. As a general rule, respirators function by filtering out harmful material before it enters your lungs while masks keep you from spreading infectious agents to others.
English physician Julius Jeffreys first patented the respirator for the treatment of chronic throat and lung diseases in 1836. Made of silk, leather, and layers of wire mesh, the respirator trapped heat and moisture. This served to loosen the mucus membranes and provided a comforting insulation from the cold, allowing the wearer to breathe more easily.
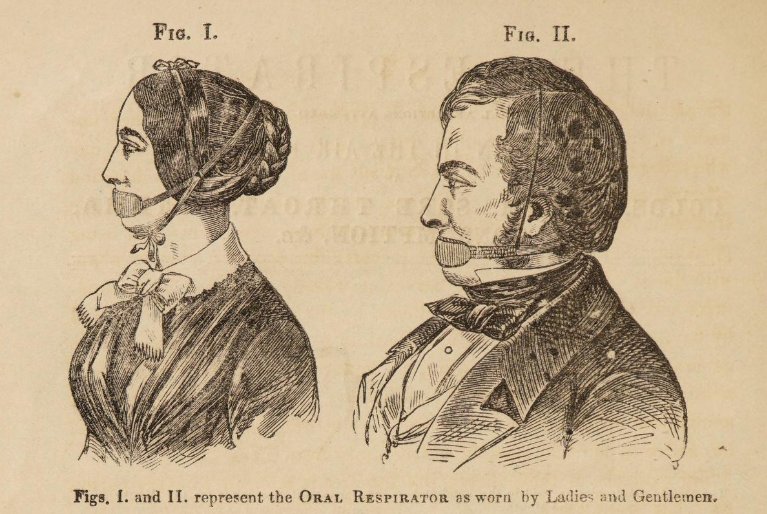
Jeffreys's Respirator advertisement, 1851.
Jeffreys began his medical career in India, where he observed that the extreme heat and humidity of lowland Bengal took a physical toll on the soldiers and officials of the East India Company. Upon returning to England, he observed that Europe’s colder, drier climate seemed to contribute to his sister’s severe asthma symptoms.
Jeffreys’s respirator provided a means of engineering what he referred to as “a local artificial climate” to open air passages in the throat and lungs. Jeffreys was so deeply committed to climate’s role in disease that he rebranded his respirator as a “climatic apparatus” in 1864.
His respirator was advertised directly to consumers and became immediately popular with the British public. Victorian writer Jane Welsh Carlyle adored her respirator. In a letter to her mother, Carlyle claimed the device had “the property of making all the air that goes down one’s throat as warm as summer air.” Despite its odd look (roughly resembling a dog’s muzzle), Jeffreys’s invention clearly had a therapeutic effect.
Jeffreys’s assertion that climate was responsible for disease was controversial. Many adhered to the belief that disease came as result of airborne poisons from the decomposition of human and animal waste. Miasma theory held that diseases drifted through these malodorous clouds and periodically afflicted populations with diseases like cholera.
Filtering these gases became the principle for a new kind of respirator. The “Inhaler” or “Lung Protector” was first patented by American Lewis Haslett in 1847. Scottish chemist John Stenhouse developed his own charcoal respirator shortly thereafter. Stenhouse had studied the use of charcoal as a means to filter toxic gases from London’s sewer systems.
Fitted to the face, the charcoal respirator was designed to adsorb harmful particles suspended in air, protecting the wearer from miasmatic illness. Stenhouse’s filtration approach gradually superseded Jeffreys’s design and formed the basic principle of the contemporary purifying respirator. Unlike Jeffreys, Stenhouse refused to patent his invention and vowed to make his innovation available to everyone at the lowest possible price.
The emergence of the germ theory of disease later in the nineteenth century superseded the miasma theory. After experiments by Louis Pasteur and Robert Koch, among others, it became increasingly clear that diseases were caused by microscopic pathogens.
The emergence of the germ led to a gradual decline in the use of the respirator as a health aid for the public at large. However, germ theory helped to usher in the widespread use of cloth masks.
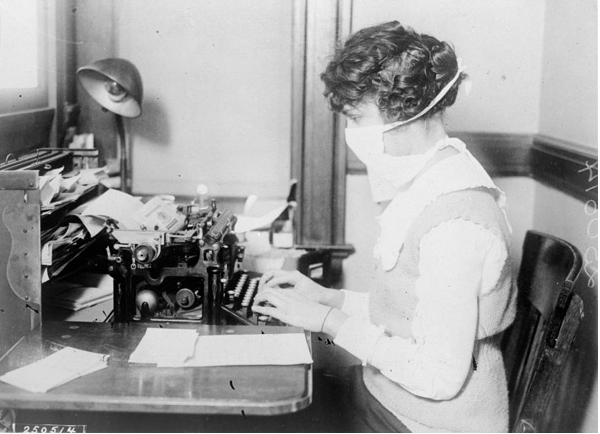
Studies of human saliva showed a multitude of bacteria capable of being spread to patients by doctors performing surgery. Simpler than the Victorian respirators, cloth masks proved effective in stopping the spread of infection when used by doctors.
Cloth was used for makeshift masks during the Third Plague pandemic in China in 1911. Evidence showed that cloth covering could prevent the spread of the pneumonic plague through coughs. The Spanish Flu of 1918 saw wide use of cloth masks around the world to prevent infection through the control of droplets emitted by coughs and sneezes.
Respirators did not disappear.
The technology to filter chemical contaminants eventually developed into the gas masks of World War I. Over the twentieth century, gas masks were called upon to filter all manner of harmful particles encountered on the battlefield environment resulting in CBRN (chemical, biological, radiological, nuclear) or NBC (nuclear, biological, chemical) personal protective equipment (PPE). Personal filtration was also widely employed in the mining and chemical industries.
The N95 respirator, which has been much in the news recently, became the industrial filtration standard in the 1970s, rated to filter 95% of harmful particles. The N95 uses polypropylene fibers to filter the COVID-19 virus suspended in air within hospital wards and other high-risk areas. These respirators must be regularly replaced to be effective. Columbus, Ohio-based company Battelle has recently developed means to safely decontaminate and reuse N95 respirators utilizing ultraviolet light.
The everyday cloth mask is not primarily intended to filter the environment outside, but rather serves as a simple means to keep the source of disease inside the wearer thus preventing its transmission to others.
The cloth mask’s role is essentially droplet control. By keeping sneezes, coughs, and other liquids confined to oneself, the cloth mask allows the wearer to breathe while creating a barrier preventing the virus to move to other hosts. Studies have consistently shown that even the modest cloth mask has a significant effect in preventing the spread of respiratory diseases to others.

A member of the US Navy wearing an N95 respirator (left). A National Guardsman sews a cloth face mask. (right).
The best way to mitigate the problem of COVID-19 continues to be social distancing. However, our networks of infrastructure, supply, and distribution are deliberately designed to bring people together in confined spaces. The efficiency gained from concentrating human beings on public transport, in warehouses, and offices now works to help the coronavirus spread.
Many cannot work from home and must place themselves at risk. So until a vaccine is developed, it is essential that those exposed to the virus—like health care workers—continue to wear respirators while the rest of us need to wear our masks to keep the disease from spreading to others.



