Vaccinations have been a triumph of modern medicine and public health. Across the globe they have reduced rates of infant mortality and contributed to increasing life expectancy. Why, then, in the 21st century would there be a significant backlash against vaccinations, even as measles and polio have re-appeared in places where they had been eradicated? This month, historian Jim Harris examines the deep roots of the anti-vaxxer movement and shows that for almost as long as there have been vaccines there have been people who oppose them.
Measles is a scary disease that is particularly dangerous to infants and children under 5. Its symptoms include high fever, cough, runny nose, and watery eyes. The characteristic rash appears a few days after the initial onset of symptoms. Measles often causes severe complications, including pneumonia and encephalitis (swelling of the brain), that can cause permanent deafness, brain damage, or neurological damage.

Infant in 1978 with skin lesions, indicative of hereditary rubella.
However, measles can be controlled through vaccination, and has been since 1963, when Drs. John Enders and Samuel Katz developed the first measles vaccine.
And we humans have succeeded at many other control efforts. By vaccination, we eliminated smallpox, one of the most dangerous infectious diseases that humans have faced, in 1980, and the World Health Organization (WHO) is edging ever closer to eradicating polio globally.
Yet as of August 2019, the U.S. Centers for Disease Control reported 1,215 individual cases of measles across 30 states this year. The vast majority of these cases (75%) have been reported in New York state. This is a shocking statistic in modern public health. The United States had declared measles eradicated in 2000, after a 22-year campaign of vaccination, and now the disease is back.
Around the world, the WHO estimates that measles is resurging even more rapidly, reporting 364,808 cases in 182 countries through the end of July 2019, including a 150% increase in cases in Europe and 900% in Africa over 2018.
The efficacy of vaccination as a tool of public health is irrefutable, not only against measles but many other highly infectious diseases as well. Thus, the Infectious Diseases Society of America, the American Medical Association, and the American Academy of Pediatrics all support the elimination of all nonmedical exemptions for childhood vaccines.
In spite of this certainty, we are seeing an increase in resistance to the use of this essential public health tool in some communities here and around the world. Why?

Anti-vaccination movements have existed for just as long as the practice of vaccination and have had complex and varied rationales. Over the past three centuries, resistance to vaccination has emerged out of ethical/theological debates, concerns about government overreach, and most recently (and most insidiously), out of a skepticism of science beginning in the 1990s.
The confluence of these factors over a long history has created a new medical crisis: the resurgence of diseases that should be eradicated through the proven practice of vaccination. Perhaps the story of vaccination development—a process that has not been perfect, but which has been progressive for human, especially childhood, health—will help remind us of why vaccination is so important to modern humans.
Smallpox and Inoculation
Smallpox, like measles, is a dangerous disease that scarred children with its characteristic “pox mark” rash. Sometimes fatal, it has plagued humans since the beginnings of recorded history. Smallpox is central to the origins of vaccination.

Bangladeshi girl infected with smallpox rash over her entire body in 1973.
Before the 18th century, Western treatments ranged from controlling the patients’ temperatures through heating and cooling to more painful treatments such as piercing the pustules with a golden needle then cauterizing them to prevent the spread of scarring.
Non-western medical traditions, however, adopted a different approach. As early as the 11th century, Chinese doctors began exposing children directly to smallpox with the intent to create a mild exposure that would grant immunity. Chinese doctors blew powder collected from smallpox scabs into the child’s nostrils through a silver tube—into the right nostril for boys and the left for girls.
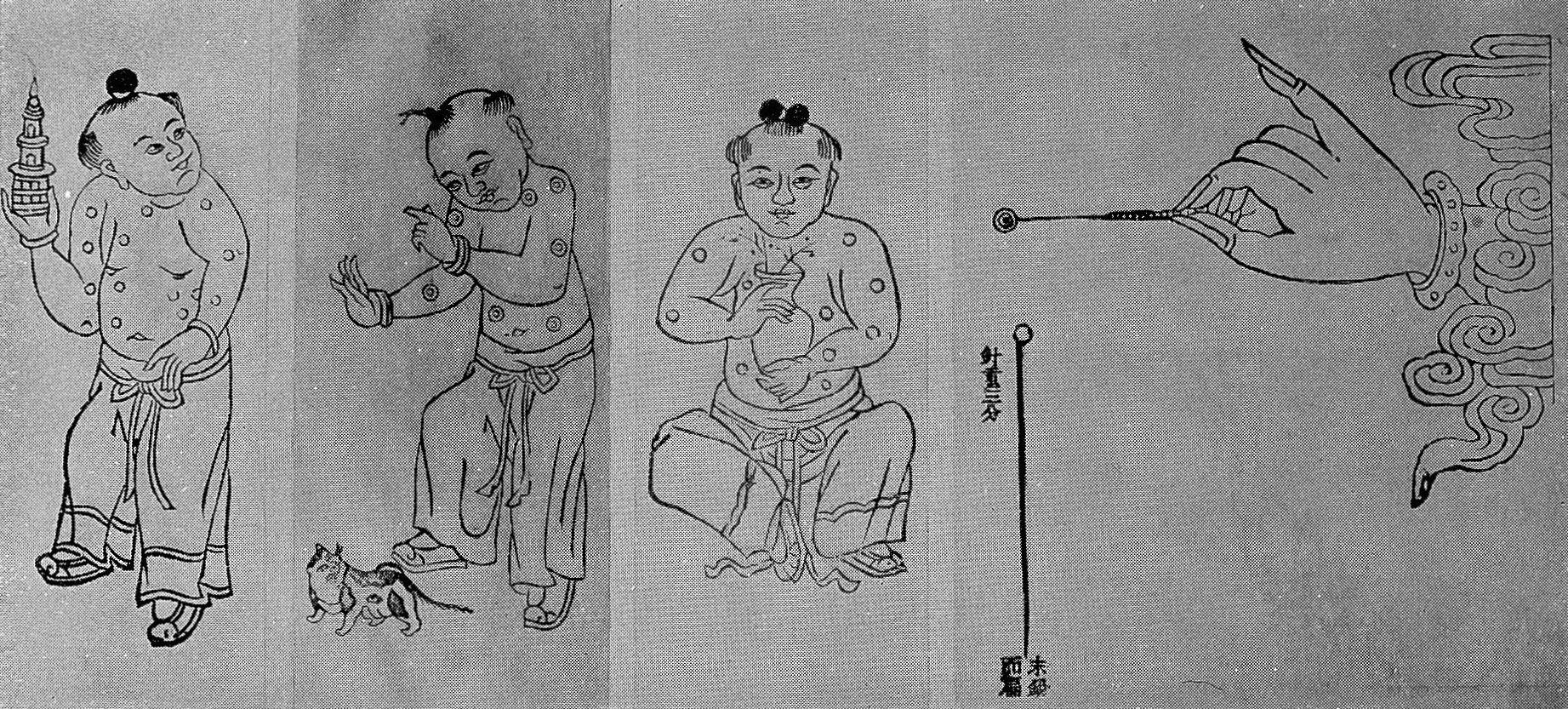
Pre-18th century Chinese vaccination method.
Such was the earliest form of inoculation, a practice that would not move westward until the 18th century when Lady Mary Montagu, wife of the British ambassador to the Ottoman Empire, observed the process of inoculation by variolation, which she described as “engrafting.” This procedure involved inserting a small amount of matter taken from a smallpox pustule under the skin of a healthy subject by way of a small incision. In most cases, the resulting infection was mild and granted lifelong immunity.
Lady Mary’s brother died of smallpox in 1713 and her own famous beauty had been scarred by the disease in 1715, so she was eager to spare her children its ravages. Thus in March 1718, she had her young son, Edward, inoculated by variolation. After her return to London, with the help of the former embassy surgeon Charles Maitland, she enthusiastically promoted the procedure by having her 3-year-old daughter publicly inoculated in 1721.

Eighteenth-century engraving of Lady Mary Worley Montagu in Turkish attire.
Initially, most British doctors scoffed at the practice as an “oriental” folk treatment practiced by peasant women rather than professional physicians. Only after Hans Sloane, president of the Royal College of Physicians, took an interest in inoculation as “an experiment of great consequence to mankind” did the path open for serious use of smallpox inoculation in England.
However, as the practice of inoculation by variolation spread through England and its colonies, new resistance to the procedure emerged. Perhaps the most notable example occurred in Boston, MA during a 1721 smallpox epidemic.
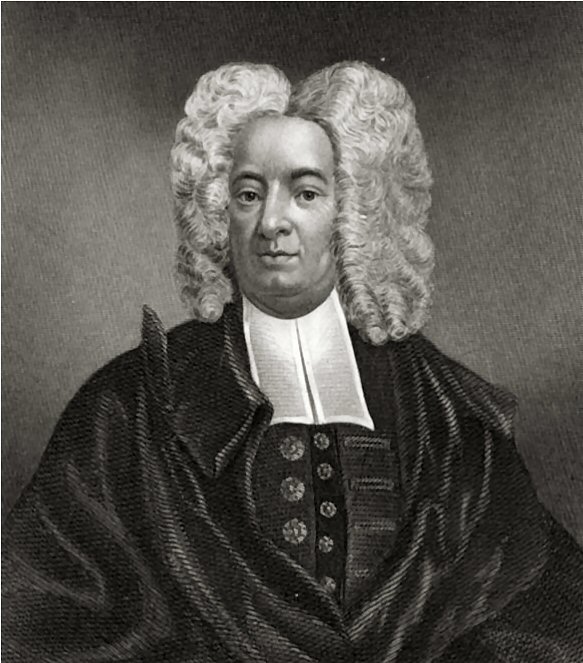
American clergyman, Cotton Mather, circa 1700.
Local Congregationalist minister Cotton Mather (1663-1728), who had studied medicine as younger man, vigorously advocated the use of inoculation, but few Boston physicians were willing. Only one of Boston’s 10 physicians, Zabdiel Boylston, was willing to take the risk.
Other Boston physicians, such as William Douglass, condemned the practice and Mather as at best “dubious” and at worst “Wicked and Felonious.” Inoculation was attacked as an affront to God’s will—for only God should determine the natural order of who might be exposed to smallpox and survive or die.
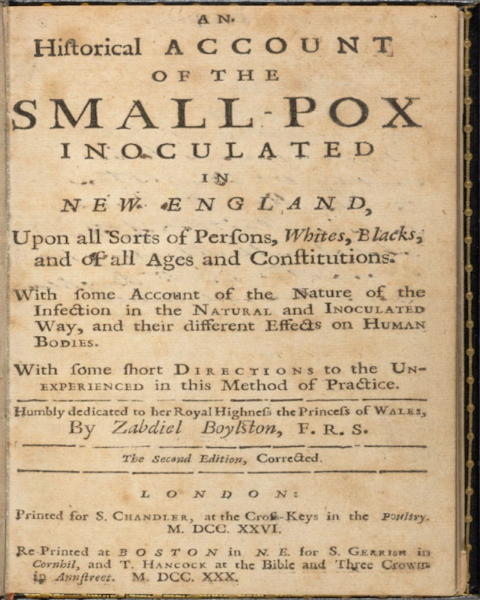
Thus the earliest resistance to vaccination (or more accurately its predecessor, variolation) was grounded in “oriental” and cultural prejudice and in religion.
From Inoculation to Vaccination
In spite of initial resistance, inoculation by variolation, using the smallpox material as the vaccine material, continued to grow over the course of the 18th century. On May 14, 1796, an important experiment would mark the origin of “vaccination” itself.
Edward Jenner (1749-1823) was a country doctor practicing in his home village of Berkeley in Gloucestershire, England. As a child he had been inoculated by variolation—a procedure he would remember as horrible throughout his life. Still, variolation was a part of his duties as a country doctor, using the same arm-to-arm system that had become common over the course of the century.
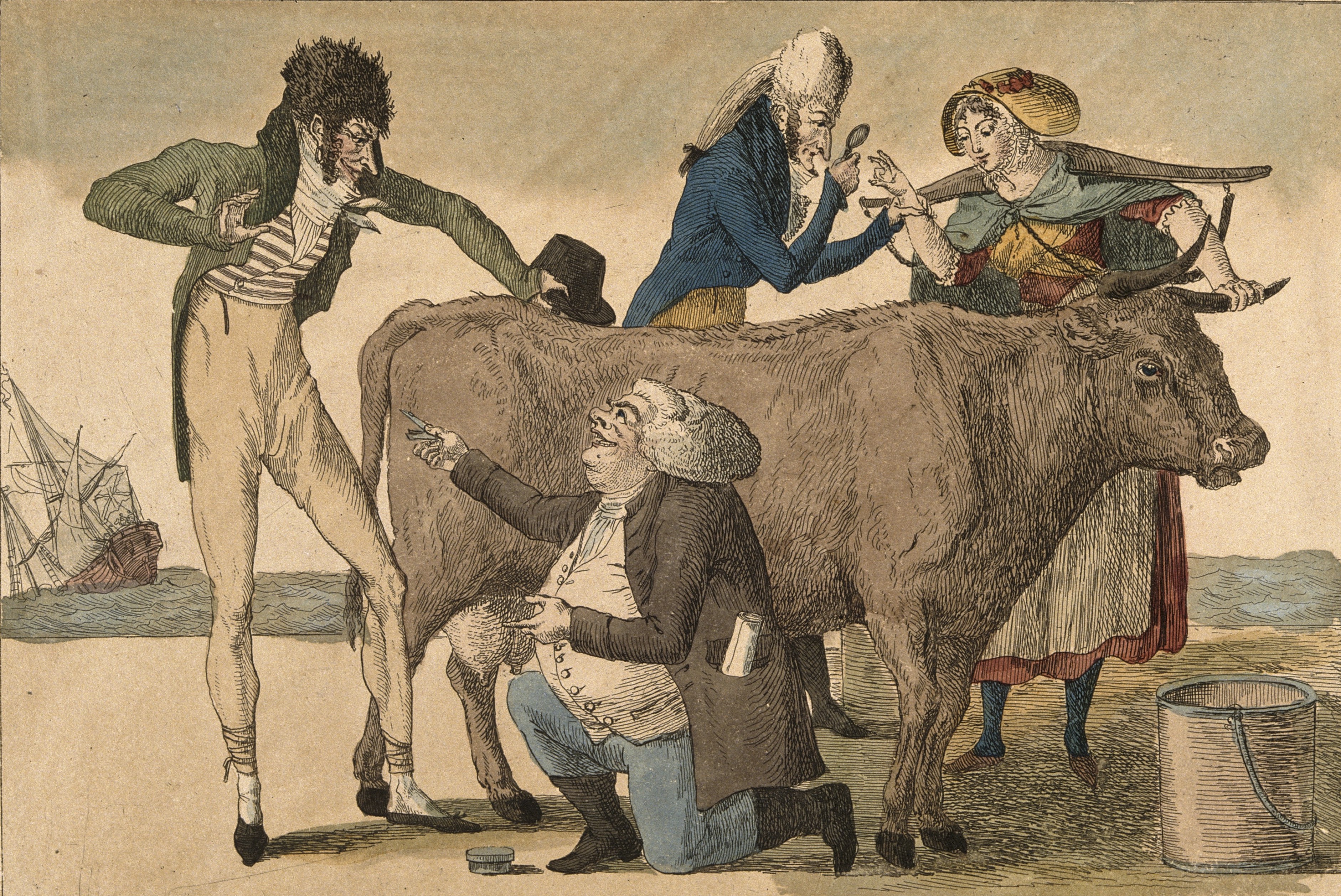
During his practice, however, Jenner made a curious discovery: milkmaids showed no side effects when they were inoculated, yet they still acquired immunity. They often told him how they had caught “cowpox” from milking diseased cows. Jenner hypothesized that perhaps it would be possible to use cowpox material (a much milder disease) for arm-to-arm inoculation instead of exposing children to smallpox itself.
Drawing vaccine material from the pox marks on the arm of milkmaid Sarah Nelmes, Jenner attempted this experiment on May 14, 1796 to inoculate James Phipps. As Jenner wrote to his colleague Edward Gardner on July 19, 1796, “I was astonish’d at the close resemblance of the Pustules in some of their stages to the variolous Pustule. But now listen to the most delightful part of my story. The Boy has since been inoculated for the small pox which as I ventured to predict produc’d no effect.” The procedure worked. Phipps became immune to smallpox without having been directly exposed.

Late 19th century lithograph of Edward Jenner’s vaccination of James Phipps.
This experiment marks the historical origin of vaccination, substituting cowpox for smallpox material in the process of inoculation, with the aim of reducing the risks involved in exposing a child to a (hopefully mild) strain of smallpox for the sake of immunization. It also marks the beginning of the use of the word “vaccine” which derived from the Latin vaccinus, from vacca (cow). It is the word we use today, whether or not cows are involved in the process.
Debates raged about Jenner’s new vaccine among London doctors.

Gillray’s 1802 caricature of vaccinated men and women growing cow parts on their bodies.
Images such as James Gillray’s 1802 painting “The Cow-Pock—or—the Wonderful Effects of the New Inoculation” helped fan the flames, illustrating apparent mutations that using cowpox to vaccinate could create. John Birch, a surgeon at St. Thomas’s Hospital, announced vaccination was useless and would allow smallpox to “recur in all the terrors with which it was first surrounded.”
Meanwhile Jenner’s supporters came to his defense.
John Ring published a 1,040-page defense of vaccination in 1801. John Lettsom, a defender of inoculation of the poor, similarly wrote of the good work of vaccination. Evangelical preacher Rowland Hill spoke of vaccination as a good cause and vaccinated thousands himself.
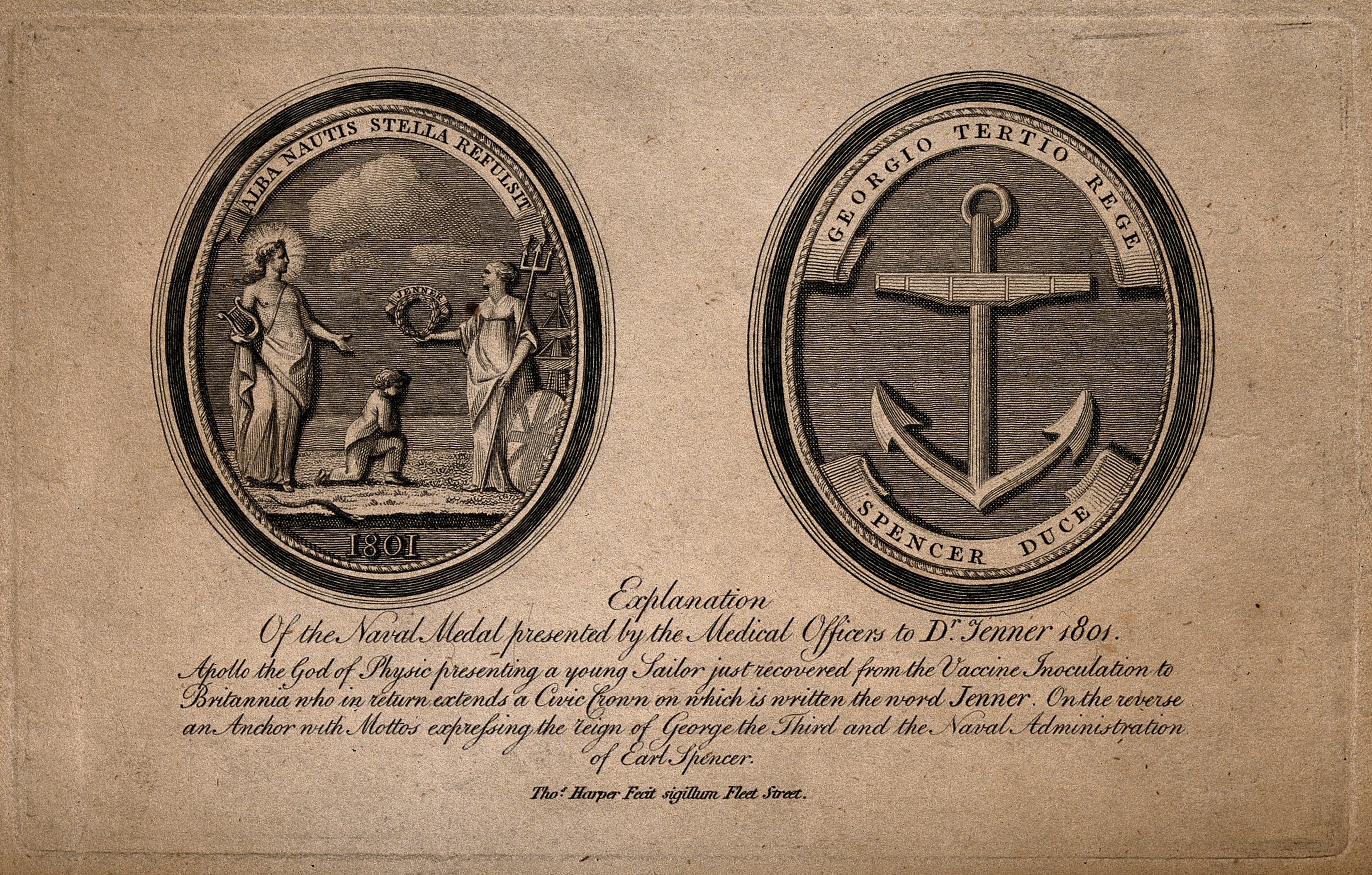
Front and back of a medal presented by British naval medical officers to Edward Jenner in 1801.
In 1802 Jenner was invited to become a member of the American Academy of the Arts and Sciences by John Quincy Adams and in 1803 Harvard granted Jenner an honorary degree for his vaccine. On May 16, 1806, Thomas Jefferson wrote to Jenner, “You have erased from the calendar of human afflictions one of its greatest … Yours is the comfortable reflection that mankind can never forget.”
Vaccination Legislation and Organized Resistance
By the mid-19th century, Jenner’s vaccine had replaced the practice of using smallpox vaccine material almost entirely with cowpox. The widespread use of vaccination dramatically reduced smallpox mortality rates. As a result, by the 1840s, Germany and the United Kingdom adopted state-sponsored vaccination campaigns.
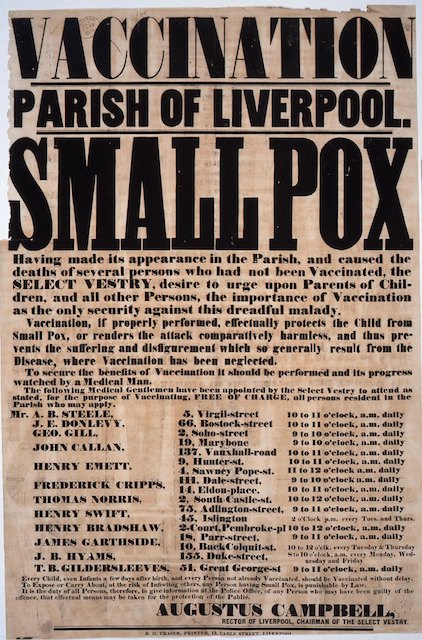
British poster urges people to get free vaccinations at specific locations in Liverpool in 1851.
In 1853, the United Kingdom passed the Vaccination Act, which mandated vaccination of infants by four months of age. If parents failed to comply, they were subject to prosecution and fines. When smallpox mortality rates rose again in the 1860s, further legislation expanded compulsory vaccination. The second Vaccination Act (1867) increased the punishment for failure to vaccinate one’s children to repeated fines and even the possibility of imprisonment.
The United States adopted compulsory vaccination more slowly, and initially on a state-by-state basis. In 1855 Massachusetts became the first state to require public-school children to be vaccinated. By the 1890s, most states had adopted similar compulsory policies.
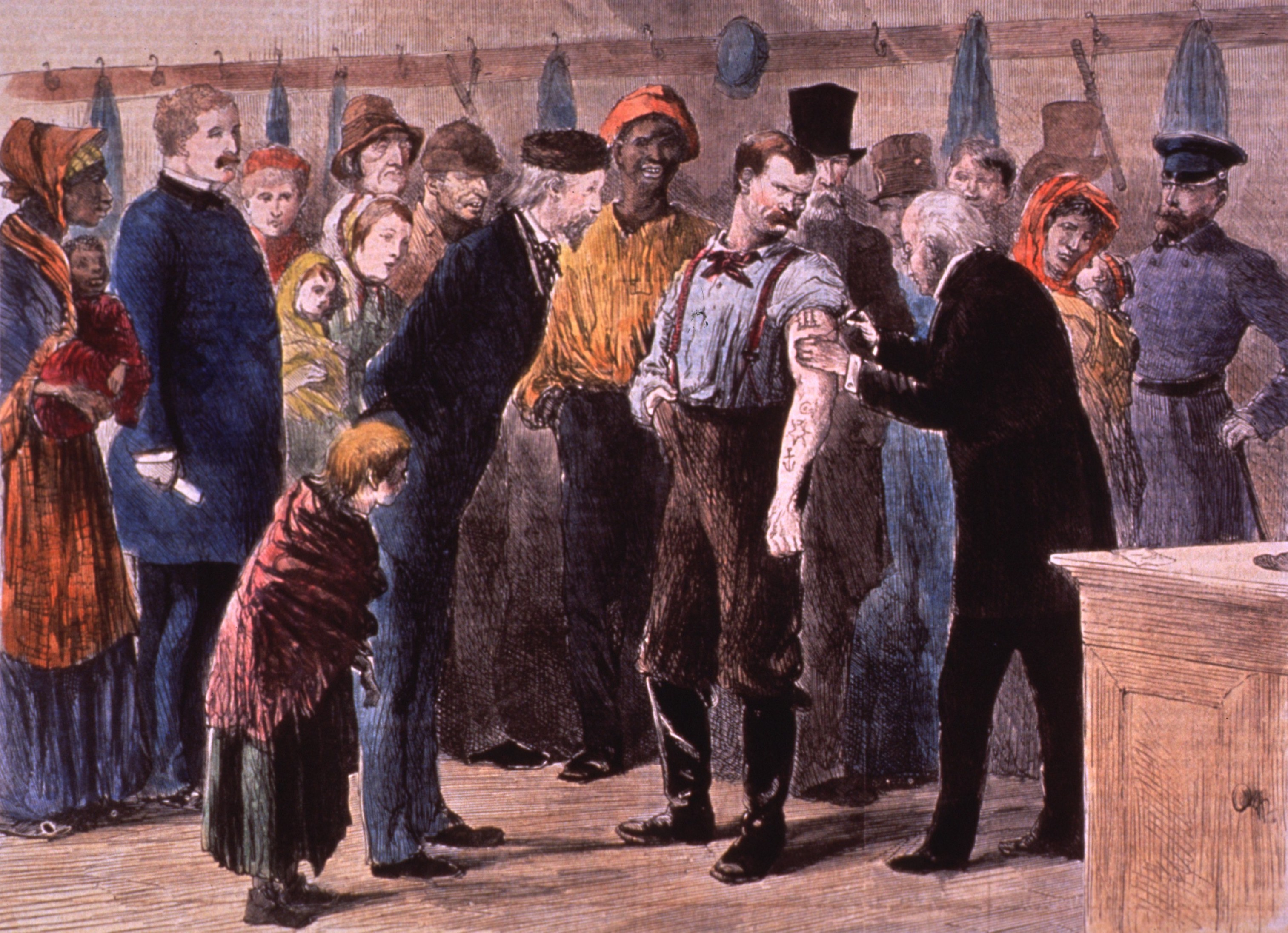
Artist’s interpretation of American public vaccinations in 1873.
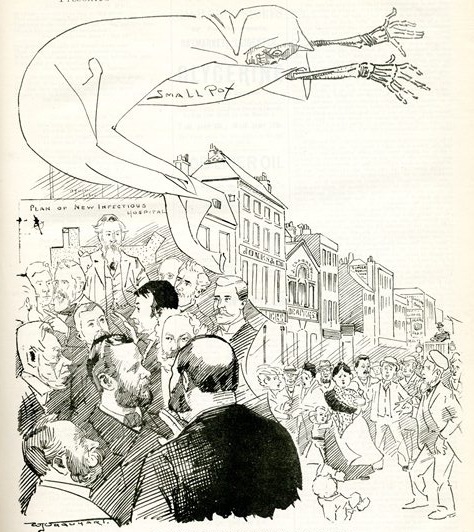
Although compulsory vaccination reduced smallpox mortality, it was met with significant resistance in both the United Kingdom and the United States. By the nineteenth century, anti-vaccination movements became primarily rooted in questions of civil liberty and the perception of government overreach.
A number of anti-vaccination societies emerged on both sides of the Atlantic, including the British Anti-Vaccination League of London (1853) and Anti-Compulsory Vaccination League (1867). In the United States, the Anti-Vaccination Society of America (founded in 1879) was the first of many such organizations to coalesce across the United States.
Advertisement to join Anti-Vaccination Society of America in 1902.
Through pamphlets, protest marches, and propaganda, anti-vaccination organizations in the United Kingdom called into question everything from the ethics of vaccination, as the procedure of arm-to-arm vaccination left visible and permanent scarring, to the safety of the vaccine material. While British elites could pay private doctors to vaccinate their children, poor Britons were forced to use a public vaccinator who sometimes vaccinated with reused vaccine material. A single sample of vaccine material could be used on hundreds if not thousands of patients.
In the city of Leicester, in March 1885, between 80,000 and 100,000 people marched to protest the prosecution of 4% of the city’s residents for failure to vaccinate their children. Demonstrators raised banners, a child’s coffin, and an effigy of Jenner.
After the Leicester protest, a royal commission was appointed to investigate the anti-vaccination grievances as well as to hear evidence in favor of vaccination. The commission sat for seven years, hearing extensive testimony from opponents and supporters of vaccination. Its report in 1896 concluded that vaccination protected against smallpox, but as a gesture to the anti-vaccinationists it recommended abolishing cumulative penalties.
In 1896 yet another Vaccination Act was passed, which eliminated these penalties, and a further Vaccination Act (1907) allowed an exemption for any parent who made a statutory declaration that he confidently believed vaccination would be detrimental to the health of the child.
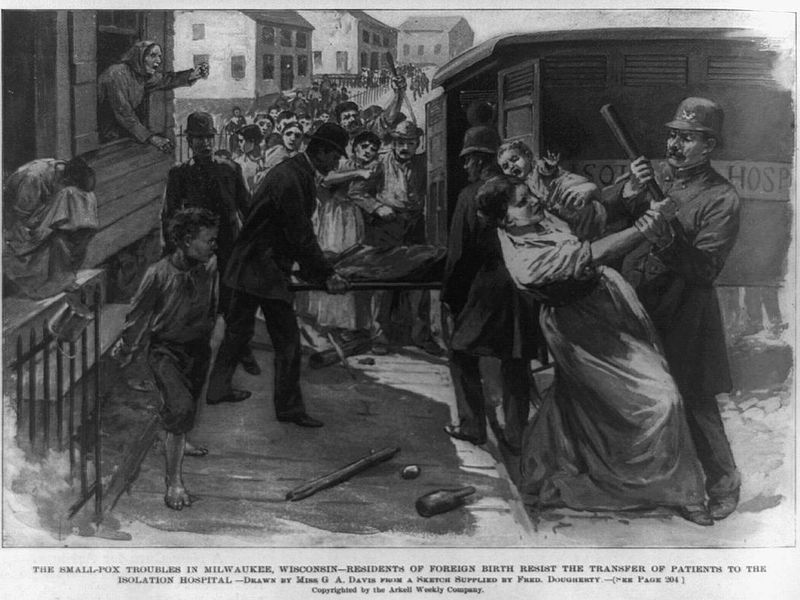
In the United States, the anti-vaccinationist movement, using pamphlets, court battles, and fights in state legislatures, succeeded in repealing compulsory vaccination laws in California, Illinois, Indiana, Minnesota, Utah, West Virginia, and Wisconsin.
However, in the landmark Jacobson v Massachusetts (1905), the Supreme Court ruled that “the state may be justified in restricting individual liberty … under the pressure of great dangers” to protect the safety of the “general public.”
The Jacobson decision meant that fines or other penalties could be imposed on parents who refused to vaccinate their children, but it also meant that conscientious objectors could not be forced to do so. This decision was upheld in Zucht v. King (1922), establishing that vaccination could be required for school attendance.
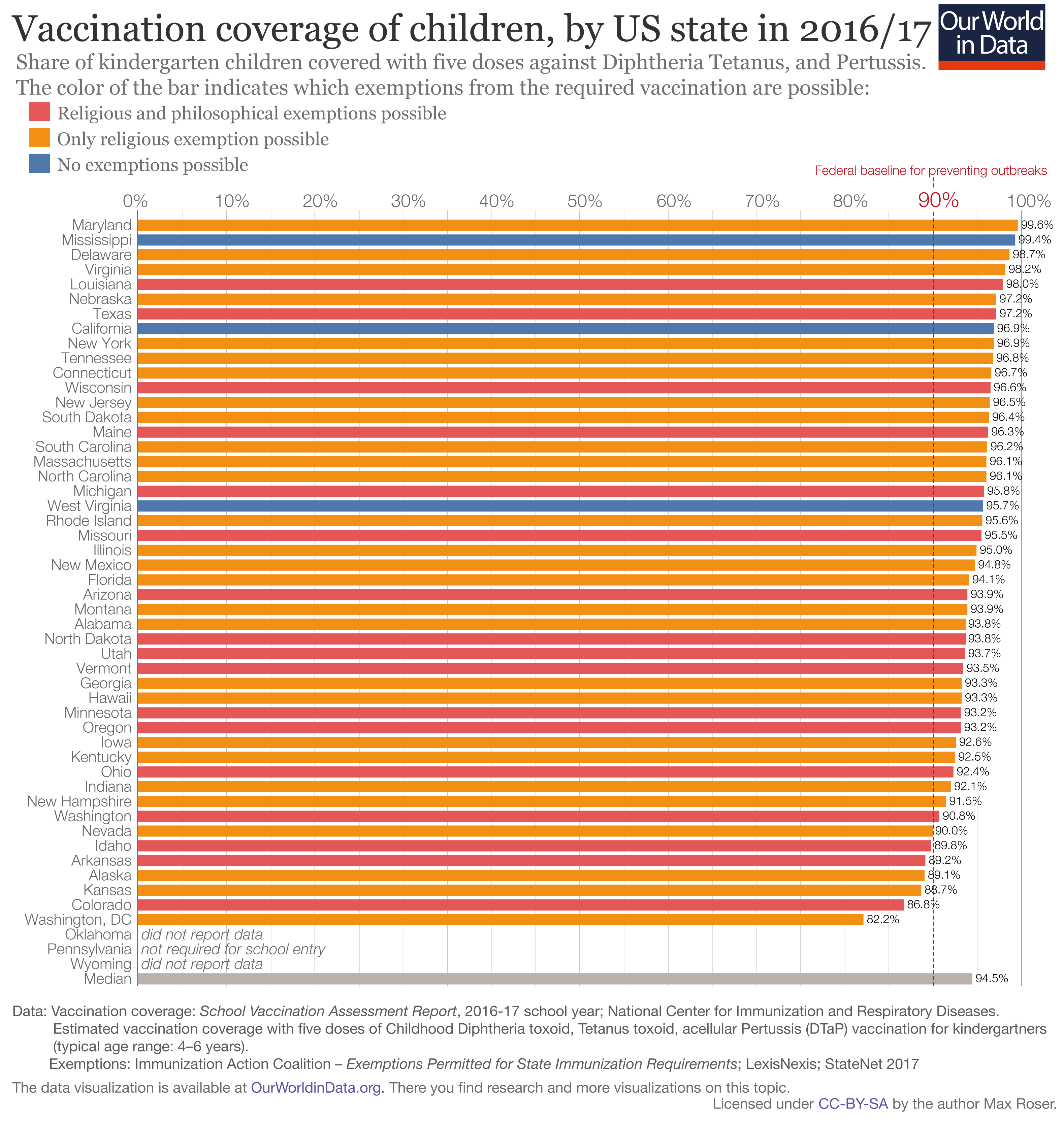
Vaccination rates and exemption status of American children 4-6 years old from 2016-2017.
The lack of coercion and emphasis on persuasion that vaccines served “the greater good” muzzled much of the anti-vaccination rhetoric (although it would remain prevalent through the 1930s), and would play an important role in launching the vaccine age in the 20th century.
Entering the Vaccine Age
In spite of organized resistance to the use of the smallpox vaccine over the latter half of the nineteenth century, its general usage and obvious reduction in smallpox mortality only invited further scientific interest in developing vaccines for other dangerous infectious diseases—especially those afflicting children.
Indeed, in 1881 Louis Pasteur revised the definition of the term “vaccination” as a universal term for preventive inoculation, based in part on his own work on anthrax and rabies vaccines.
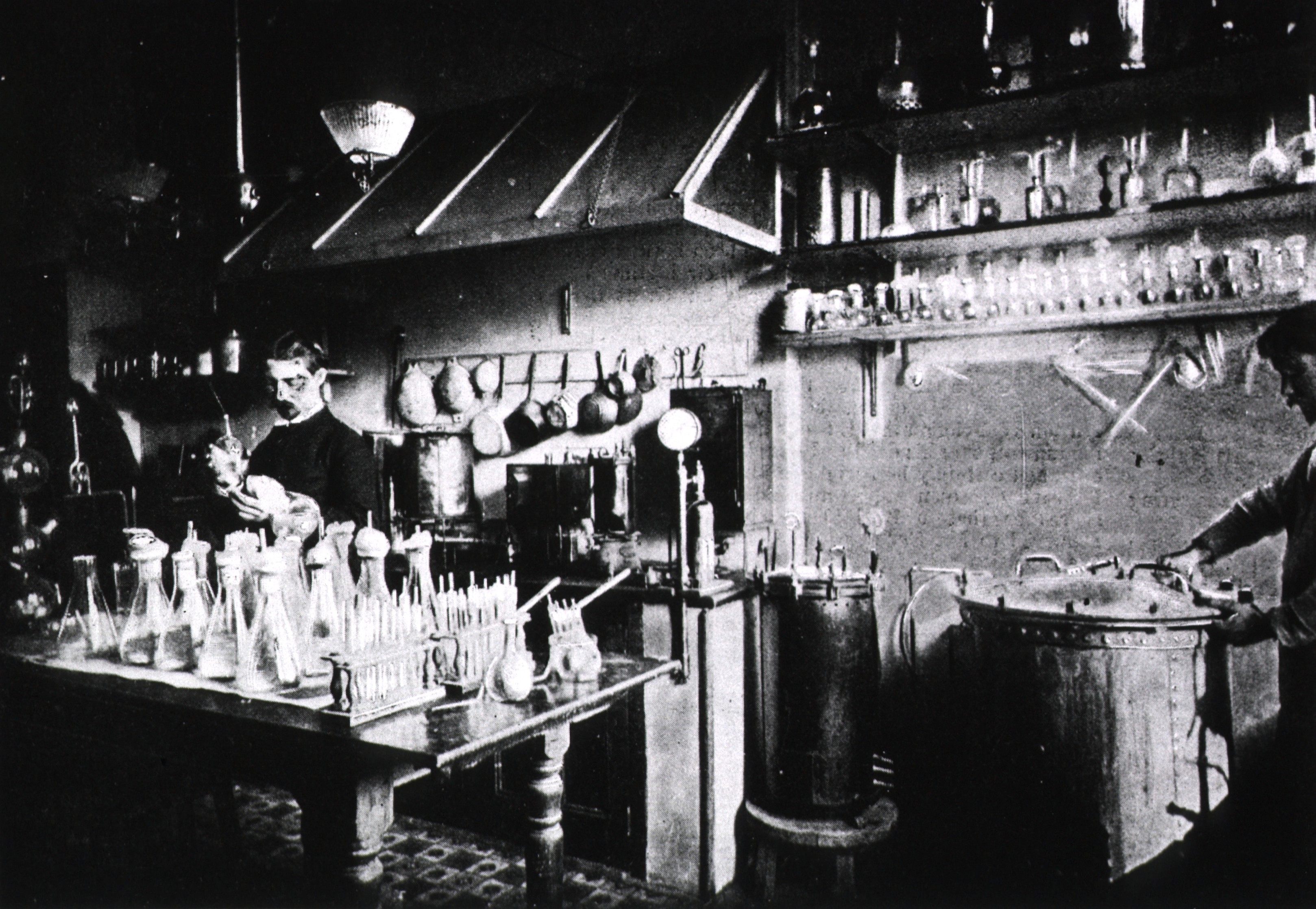
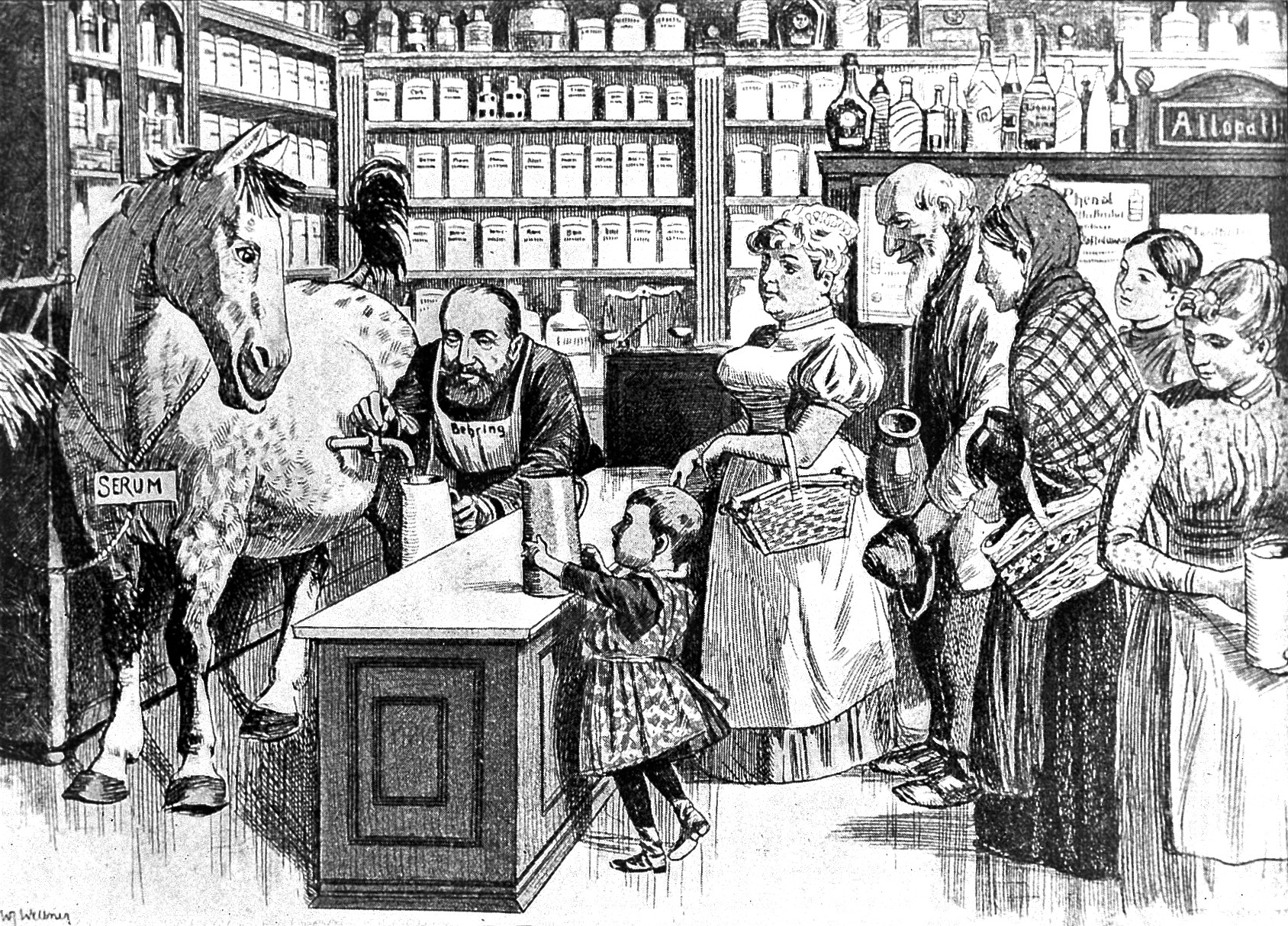
Work on a vaccine for diphtheria, a bacterial disease that killed children by sealing their throats with a thick gray “pseudo-membrane,” began in the 1890s, when most physicians were apathetic about a potential treatment. In New York City, where the disease had become the sixth leading cause of death, and particularly afflicted children under 5, the board of health ordered the use of an anti-toxin as a highly effective form of treatment.
As the use of anti-toxin was used more widely, researchers began to study how to create a proactive treatment for diphtheria. In 1907, Dr. Emil von Behring, who had already won the Nobel Prize in medicine in 1901 for his work on the anti-toxin, proposed in a paper that a mixture of diphtheria toxin and antitoxin produced safe and lasting immunity in humans.
In 1914, Dr. William H. Park of the New York City Board of Health began clinical trials of a mixed toxin-antitoxin vaccine in animals and then in human trials to find the precise balance necessary to create lasting immunity without a reaction to the mixture.
The vaccine was first widely used in 1920, and then replaced in 1923 with an improved (heat-treated) toxoid vaccine developed by the Pasteur Institute in Paris. The results were a precipitous drop in diphtheria mortality by the late 1920s. In 1948, the diphtheria vaccine was combined with a vaccine for tetanus and pertussis (whooping cough) as the DTP vaccine.
The first documented case of polio in the United States occurred in 1894, but a 1916 outbreak of approximately 27,000 cases and 6,000 deaths brought national attention to the disease. As the therapeutics for polio were limited and invasive, to say nothing of the stigma that patients faced, work on a vaccine began as early as 1935, when Maurice Brodie at NYU attempted to develop a vaccine from monkey spines. His vaccine failed disastrously in clinical trials, killing several patients and paralyzing many others.
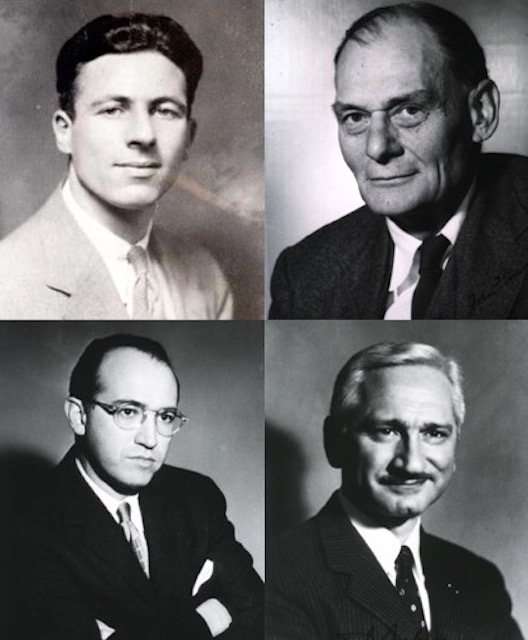
Maurice Brodie (top left); John Enders (top right); Jonas Salk (bottom left); Albert Sabin (bottom right)
The real challenge in studying the polio virus to develop a vaccine resulted from the difficulties in culturing virus samples. Dr. John Enders and his team at Boston Children’s Hospital overcame this hurdle, showing how to culture the virus in human muscle tissue in 1948. They received the Nobel Prize in medicine in 1954 for this discovery.
Using Enders viral cultures, Dr. Jonas Salk at the University of Pittsburgh Virus Research Lab was able to develop a “killed” virus strain that could elicit an immune response in humans. Salk’s lab began a nationwide clinical trial in school children in April 1954 and the results were positive: 60-70% prevention.
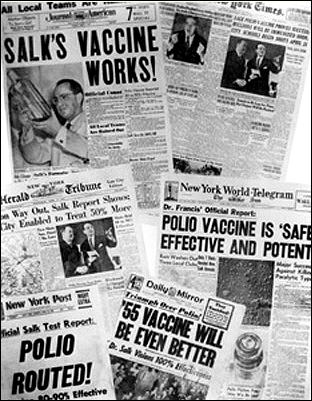
Newspaper headlines from 1955 about polio vaccine and Dr. Jonas Salk.
But this still left a large percentage of children at risk.
Dr. Albert Sabin, head of Pediatric Research at the University of Cincinnati, believed that a killed virus was not strong enough, so he began experimenting with a weakened “live” strain.
In 1957, he began clinical trials in the Soviet Union and in spite of its “communist” origins, the United States began to make use of his vaccine widely in 1962. It was cheaper to make and easier to take than Salk’s injectable vaccine and, despite the risks, Sabin’s oral vaccine proved to be a more natural and certain method of boosting immunity to polio.
Many of these same laboratories worked on a measles vaccine in the mid-20th century as well. As a highly contagious virus with no direct treatment and a case-fatality rate as high as 28%, measles unfortunately remains a major public health concern, especially in schools (given its resurgence since 2000).

The first measles vaccine was tested in October 1958 in Enders’ Boston lab by Dr. Samuel Katz. Twenty children were given an experimental vaccine: 11 developed antibodies, nine a measles-like rash. Enders and Katz’s first vaccine was a failure. By 1962, after a series of similar attempts, they discovered that a killed-virus vaccine did not create the desired immune response. A year later they successfully tested a safe live attenuated measles vaccine, which would undergo further improvements through the 1960s.
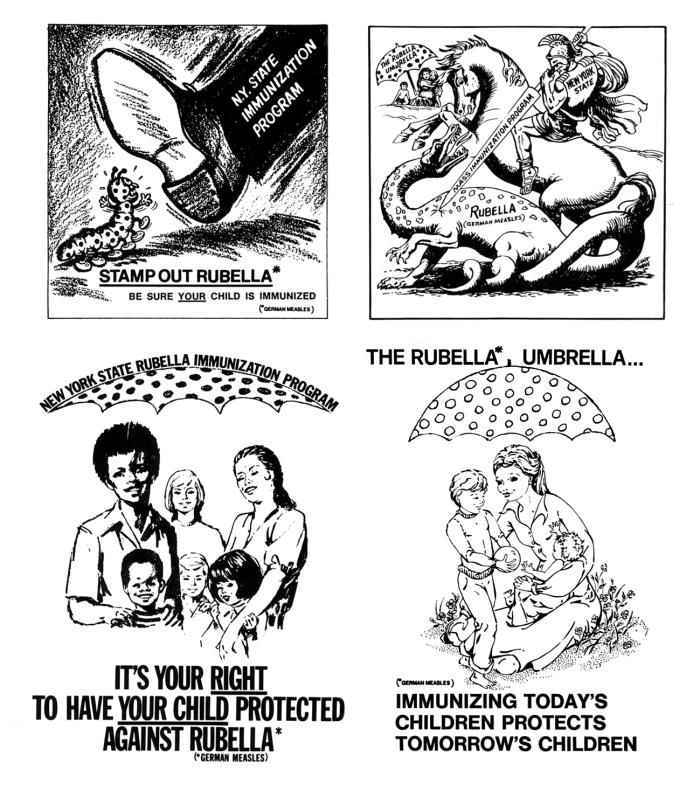
By 1971, Merck & Co. pharmaceuticals was able to develop a measles vaccine that could be safely be combined with the mumps and rubella vaccines—the modern MMR vaccine. In 1978 the CDC declared its intent to eradicate measles in the United States by 1982. They did not meet this goal, though cases of measles dropped dramatically. It was eradicated in the United States in the year 2000.
Andrew Wakefield and the Modern “Anti-Vaxxer” Movement
By the late 1980s, laws mandating immunization for children to attend public schools were solidly established across the United States. The principle that the vaccines served the “greater good” had been upheld in the courts for nearly a century in defense of this program. For those parents who could not afford childhood vaccines (about $300 in 1990), public funding programs were established in the 1990s.
Why, then, is measles resurging in the United States and around the world? The answer, in part, is because of a renewed resistance to vaccination. Anti-vaccination movements have historically been grounded in various objections—religious and civil libertarian—and those issues remain.

Hasidic Jewish family in New York in 2013.
The question of individual liberty to make medical decisions for oneself and one’s children remains complex. Similarly, theological issues continue to prevent a challenge to compulsory vaccination. In the United States, religious communities, including ultra-Orthodox Jews, continue to demand the right to a religious exemption from mandatory vaccination.
Forty-five states allow moral or philosophical exemptions from mandatory vaccination for enrollment in schools, while fives states (California, Maine, Mississippi, New York, and West Virginia) only allow medical exemptions. From a medical perspective, the right to religious exemption has no basis, yet these are still granted. The reason this exemption remains is entirely a question of faith and the subject of a debate that dates back to the 18th century.
Furthermore, the modern anti-vaccination movement has also developed a new rationale: a skepticism of the science.
In 1998, now discredited British doctor Andrew Wakefield published a paper in The Lancet, one of the most important medical journals in the world, in which he falsely reported that the Measles, Mumps, and Rubella (MMR) vaccine was linked to autism in 12 cases.
In the paper, Wakefield described a direct link between gastrointestinal disorders and the cause of autism, and noted that these disorders developed as a result of the childhood MMR vaccine. Wakefield called for the suspension of the MMR-linked vaccines, suggesting that vaccines for each disease should be administered separately to prevent gastrointestinal distress.
There is a historical precedent for Wakefield’s assault on science. In the late 1970s in the United Kingdom, the DPT vaccine (diphtheria, pertussis or whooping cough, and tetanus) was attacked by University of Glasgow physician Gordon Stewart for its rare side effects, which included permanent brain damage. The response was careful monitoring both in the Great Britain and the United States of children who had received the DPT vaccine and the results were clear.
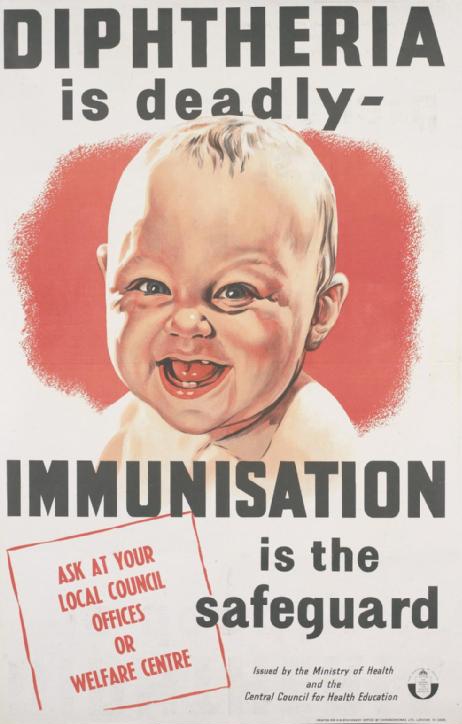
British poster created before 1945 promoted diphtheria vaccinations.
Although the DPT vaccine received considerable negative press, the ability to prevent pertussis massively outweighed the exceedingly rare side effects. Yet the histories of “damaged youth” nevertheless carved out a path to attack the science and safety of vaccine development.
In the case of Andrew Wakefield’s assertion that the MMR vaccine could be linked to autism, journalist Brian Deer found in 2004 that Wakefield had no data at all to support his claim. The paper was entirely fabricated and fraught with conflicts of interest; as Deer first discovered, Wakefield was funded by solicitor Richard Barr, who was trying to bring suit against the combined vaccine manufacturers.

Actors Jenny McCarthy and Jim Carrey, holding a photo of McCarthy’s autistic son, at a 2008 anti-vaccination rally in Washington, D.C.
The paper was not fully retracted until 2010. By then, the damage had been done. Celebrities such as actress Jenny McCarthy latched onto the claim and began promoting Wakefield’s false link between vaccination and autism. A vocal minority of anti-vaccinationists continue to espouse this belief, even though there is no scientific evidence to support it.
Other vaccine skeptics fear vaccines more broadly. Some question risks of additives such as thimerosal, a compound containing ethylmercury, added to vaccines to prevent bacterial contamination. Through extensive studies, the CDC has found thimerosal safe at low dosages.
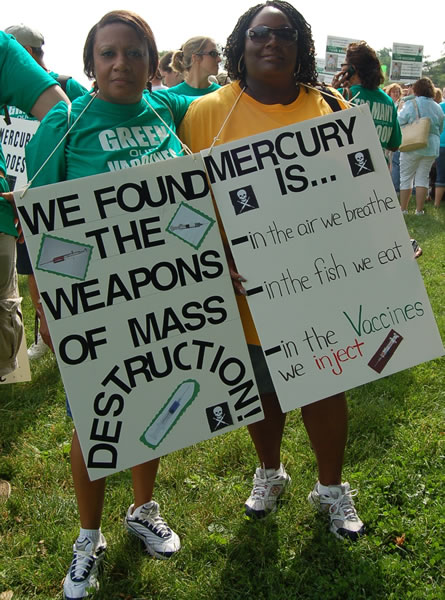
Anti-vaccination supporters at the 2008 “Green Our Vaccines” march in Washington, D.C.
Furthermore, as the history of science particularly shows, vaccines are among the most rigorously tested tools in modern biomedicine and the science has only developed further since their inception 223 years ago.
For the Greater Good
The United States must maintain a 95% vaccination rate against measles in order to maintain what is known as “herd immunity.” If a high enough percentage of people in a community are immune then the chance of disease spreading in the community drops very low and even those not immunized are protected. According to the New York Times, over the past three years this number has been gradually slipping to as low as 94.3% last school year.
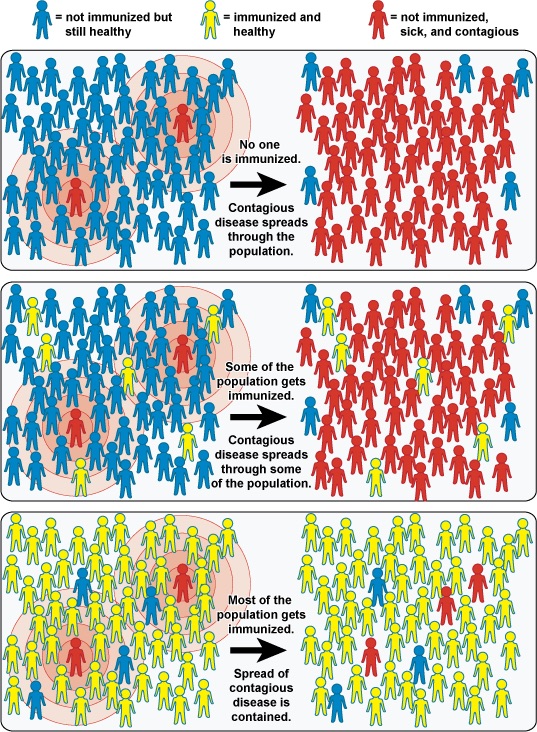
National Institute of Allergy and Infectious Diseases’ 2010 chart illustrates how vaccinations can prevent disease outbreaks.
A historical perspective can only begin to address the complex, historically profound ethical questions about vaccination—questions that are tied to religious rights, civil liberty and the role of group thinking in the internet age.
However, the science is clear: vaccines work. They must be deployed to preserve public health in the name of the greater good, as Jacobson v. Massachusetts argued more than 100 years ago.
Read more on Vaccination and Public Health from Origins: Vaccination; Vaccines and Parenthood; The 1918 Flu Pandemic; Flu History; A Century of HIV; Influenza Pandemics; America's Mental Health System; Veterans Health Care; and Fluoride and Public Health.
Listen to more on public health: HIV/AIDS: Past, Present and Future; Affordable Care Act; and Mental Health and American Society.
Colgrove, James. State of Immunity: The Politics of Vaccination in Twentieth-Century America. Berkeley: University of California Press, 2006.
Durbach, Nadja. Bodily Matters: The Anti-Vaccination Movement in England, 1853-1907. Durham: Duke University Press, 2005.
Glynn, Ian and Jennifer. The Life and Death of Smallpox. London: Profile Books, 2005.
Mnookin, Seth. The Panic Virus: The True Story Behind the Vaccine-Autism Controversy. New York: Simon & Schuster, 2011.
Oldstone, Michael B.A. Viruses, Plagues & History: Past, Present, and Future. Revised and Updated Edition. Oxford: Oxford University Press, 2010.
The College of Physicians of Philadelphia. The History of Vaccines. 1787. https://www.historyofvaccines.org.
Willrich, Michael. Pox: An American History. New York: Penguin, 2011.

