The three decades or so after World War II witnessed the greatest assault on infectious disease in human history. The newly formed World Health Organization (WHO), in collaboration with governments all over the world, marshaled unprecedented resources to control and, in some cases, to eradicate infectious diseases.

Key to this sustained attack were a series of medical breakthroughs. Antibiotics, effective vaccines, and insecticides like DDT were among the most important. But without the will and commitment on the part of governments, health care professionals, the general public, and the WHO the mere presence of effective medical technology would not have been enough to control or defeat disease.
The optimism, ambition, and, yes, hubris, that characterized the postwar push to control infectious disease was tempered by the reality of the fragile public health infrastructure found in many places where the WHO operated mass vaccination and eradication campaigns.
Thus, while the postwar spirit and determination should be applauded—and even, one can hope, emulated in our time as we watch the lackluster performances of governments and people in response to Covid-19—we must be also be mindful that a robust public health infrastructure is essential to the success of any large-scale infectious disease program.
In the early 1950s, the WHO targeted tuberculosis (TB) and launched what it called the “largest mass action the world has ever known against one single disease.” In 1953, the doctor who carried out the WHO’s first African TB survey wondered in amazement at “how much the Organization and the world in general would profit scientifically and practically from such work in the ‘terra incognita’ of Africa.”
TB control on such a scale was entirely new and it happened fast—perhaps too fast. The effort to control the disease moved at such a pace that, in the words of the director of the Eastern Mediterranean Office of UNICEF (the United Nations Children's Fund), “organizational success has been so great that it has been difficult for the progress in knowledge and technique to keep pace with this development.”
Moving quickly into places not ready to take full advantage of medical technology and public health initiatives, however, was not limited to TB control nor has it gone away. It has been a feature of malaria control efforts for generations: from the WHO’s malaria eradication program, launched in the 1950s and over by the late 1960s, to the more recent Roll Back Malaria campaign. These programs to control the disease have been foisted upon places unable, because of weak health systems, to implement them properly.
The postwar push to control TB was part of a larger effort to control all infectious diseases after the war. During the 1950s and 1960s especially, there was a buzz in the air about disease eradication and wonder drugs.

Tuberculosis Hospital in Seoul, South Korea, 1952.
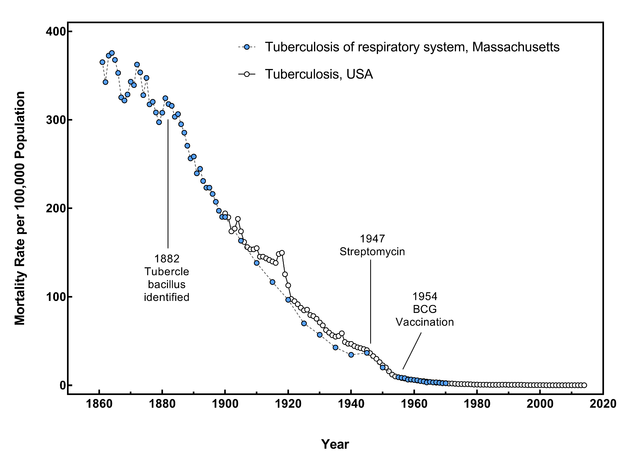
In 1952 Selman Waksman won the Nobel Prize in 1952 for his work discovering streptomycin, an antibiotic that could cure TB. And there was tremendous excitement over TB’s new miracle antibiotic, isoniazid, in the early 1950s. Was it now time, some people asked, to cheer the death of TB?
This was the climate in which infectious disease specialist T. Aidan Cockburn claimed in Science in 1961 that “we can look forward with confidence to a considerable degree of freedom from infectious diseases at a time not too distant in the future.” William Stewart, the Surgeon General of the United States, is even said to have claimed in the late 1960s that “it is time to close the book on infectious diseases, and declare the war on pestilence won.”
There was such optimism about the power of biomedicine that some believed medical technology would foment the leap from primitive society to modern civilization.
A biomedical engineering experiment, conducted at Rice University, 1969.
Walsh McDermott, a prominent TB and international health expert noted in 1963 that biomedical research and interventions were crucial to what he called “planned modernization.” By making formerly sick people well they could then become productive citizens. They would learn the benefits of modern, preventive, medicine.
According to McDermott, because of antibiotics the control of TB, in fact, “is one of the few instances to date in which a major disease can be decisively altered without having to await improvement in the social infrastructure” [emphasis added].
In 1962, Fred Soper—famous for his efforts to eradicate malaria—declared that TB could be wiped off the face of the earth. When people finally accepted that TB “was no longer a social and economic but rather a public health and medical administrative problem,” Soper wrote, it could be done away with.
But controlling infectious diseases is not so simple.
On the ground and in the field, TB workers were cautiously optimistic at best. They were not dazzled into thinking the promise of new drugs would make “primitive” people “modern” or that the technology of TB control would tackle poverty. Rather, in the face of drug resistance, escalating rates of TB, and cost, they often appear frustrated with the lost promise of medical technology.
The European director of UNICEF declared in 1962 that establishing “adequate tuberculosis control programs in these developing countries is no more than a dream, since even the most rudimentary organization for public health protection is lacking, and that tuberculosis control in these countries can only considered within the framework of more broadly based and strengthened public health services.”
And this remains the problem right down to the present: life-saving drugs are only as useful as the public health system within which they exist.

Reflecting pool at the World Health Organization Headquarters, 1962.
In Africa, where TB was most rampant, lack of public health infrastructure led to poorly controlled antibiotic supplies and eventually an epidemic of drug resistant TB. Despite the extraordinary campaign against the disease, a group of TB experts had this to say in 1995: “Consistently, the world community has failed even to implement those effective and well-tried measures against tuberculosis that have existed for almost 40 years.”
As we face a new pandemic of infectious disease, let’s hope we can find the will and ambition world leaders summoned decades ago. At the same time, let’s also hope that we build a public health infrastructure capable of managing an eventual vaccine or therapeutic—and maybe even a system robust enough to defend us from the next pandemic.

